[tweet][digg][stumble][Google][pinterest][follow id=”DER29709692″ size=”large” count=”true” ]
Cervical cancer is a major killer among women but doctors believe it is preventable
By Chris Ajaero
It is the most common malignancy that is of public health concern in women, especially as it affects a woman’s organ. Medical experts believe that every sexually active woman is at risk of cervical cancer. Indeed, latest statistics from the World Health Organisation, WHO, shows that Nigeria has a population of about 48 million women aged between 15 and 44 who are at the risk of developing cervical cancer. Current estimates indicate that every year, 17,550 women are diagnosed with cervical cancer and 9,659 die from the disease. Professor Ifeoma Okoye, a radiologist and founder, Breast Without Spot (BWS) Initiative, a School-Based Cervical Cancer Vaccination Awareness Initiative said recently that no fewer than 26 Nigerian women die daily as a result of cervical cancer. According to her, cervical cancer was killing more people worldwide than HIV/AIDS, tuberculosis, and malaria put together. “We conducted a survey and discovered that cervical cancer is the second killer cancer among women and Nigeria is also the tenth in cervical cancer death worldwide. Forty-eight million women are at risk, 17,550 women are diagnosed yearly, 9,659 women die annually and 26 women on daily basis in Nigeria.
“This is alarming and most of the cases are rampant in the developing countries like Nigeria. It, therefore, requires a proactive political commitment to fight the scourge,” she said
Worried by the trend, the Federal Ministry of Health of Health had some time ago, launched a free vaccination programme against the Human Papiloma Virus, HPV, which causes cervical cancer. Professor Onyebuchi Chukwu, minister of health said the launching of the free 5,000 doses of Cervarix, the HPV vaccine for indigent girls aged between nine and 15 was aimed at reducing the burden of cervical cancer cases in the country. He urged public spirited individuals and organisations to join the ministry in the battle against the scourge.
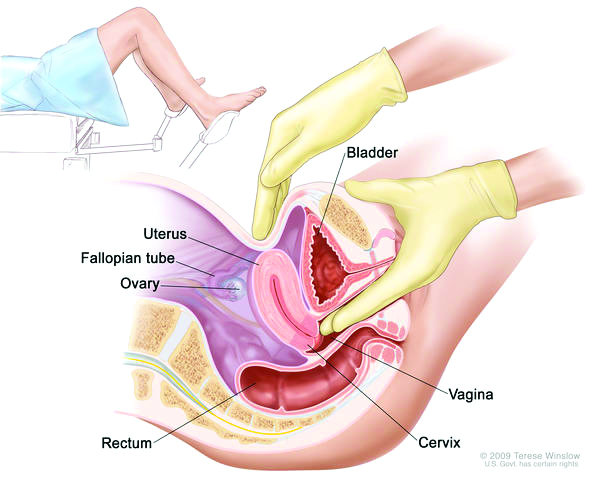
But then, what exactly is cervical cancer? Professor Remi Ajekigbe, consultant radiotherapist and oncologist, Lagos University Teaching Hospital, LUTH, Idi-Araba, Lagos said cervical cancer occurs when healthy cells in the cervix acquire a genetic mutation that turns normal cells into abnormal cells. The cervix is the lower part of the uterus or womb that opens into the vagina. According to Ajekigbe, cervical cancer is sex related because it is rare in virgins or nuns and it can occur in any woman that is old enough for sex or has been involved in sexual activities. The predisposing factors that can either increase or enhance the chances of having cervical cancer are early exposure to sex, multiple sexual partners and prostitution. Other factors include a woman who gives birth to several children, women who smoke or use oral contraceptives. In addition, genetically, if there was a family history of someone having it, her daughter could also be predisposed to the infection.
Cervical cancer is the second commonest cancer in women in Nigeria, especially in the Southern part of the country; but in some parts of the North, it is also the leading cancer. The symptoms of cervical cancer include abnormal vaginal bleeding such as inter-menstrual bleeding in between menses, post-coital bleeding, which is bleeding after sex, or post menopausal bleeding, watery vaginal discharge and offensive vaginal discharge. At an advanced stage, it is present with waste pain and abdominal swelling.
Dr. Anthonia Sowunmi, another consultant radiotherapist and oncologist at LUTH explained that because cervical cancer affects the neck of the womb, it takes people a long time to discover that there is a problem in that part of the body. According to her, sexually transmitted infection that causes cervical cancer is known as Human Papiloma Virus, HPV. The exposure or contact with this virus predisposes persons to having this cancer in future. This virus could stay for as long as 10 to 15 years in the body of a sexually active woman before it manifests. Since it takes many years for the virus to develop into full cancer and there are no early symptoms, the woman feels very healthy while the virus continues to ravage her. By the time the symptoms begin to show, the situation becomes uncontrollable.
Sowunmi identified some of the symptoms of the ailment that may appear by the time the cervical cancer has become more advanced. “What makes one suspicious of cervical cancer is that women experience bleeding after sexual intercourse which has continued for a long time, all of a sudden start noticing discharge in their private part that has an offensive odour. When this happens, it is important for the person to go for clinical examination as quickly as possible,” she said.
Sowunmi advised women who notice such symptoms to go for the test in reputable health institutions, especially the government hospitals where they have better laboratory facilities.
Experts suggest that sexually active women should regularly go to the Centre for Disease Control, CDC, located in many Nigerian teaching hospitals for screening to prevent the disease since prevention is better than cure. Such sexually active women are advised to go for screening at the age of 21, or within three years of becoming sexually active.
During a pap test, the doctor brushes cells from the woman’s cervix, which is the narrow neck of the uterus – and sends the sample to a laboratory to be examined for abnormalities. The doctor may use also use a laboratory test called HPV DNA test to determine whether the woman is infested with any of the 13 types of HPV that are most likely to lead to cervical cancer.
During a medical examination called colposcopy, the doctor uses special microscope (colposcope) to examine the cervix for abnormal cells. Tests such as x-rays, computerised tomography, CT scans and magnetic resonance imaging, MRI, equally help the doctor to determine whether cancer has spread beyond a woman’s cervix.
It is only after such tests that treatment can start. Cervical cancer that is caught early can usually be cured. Treatment for cervical cancer depends on several factors, such as the stage of the cancer, other health problems the patient may have and her preferences about treatment. The cervical cancer that is confined to the outside layer of the cervix typically requires treatment to remove the abnormal area of cells. For most women in this situation, no additional treatments are required.
However, when cervical cancer has invaded deeper than the outside layer of cells on the cervix, it is referred to as invasive cancer. This requires more extensive treatment.
Treatment options may include: surgery to remove the uterus. This is known as hysterectomy and is typically used to treat the early stages of cervical cancer. Hysterectomy can cure early-stage cervical cancer and prevent cancer from coming back. The removal of the uterus makes it impossible for the woman to become pregnant.
Before going ahead with this type of treatment, the reproductive stage of the patient would be taken into consideration. If she had concluded delivering, the entire womb and the neck can be removed.
Cervical cancer could also be treated through radiation therapy. This entails using high-powered energy to kill cancer cells. Another mode of treatment is chemotherapy. In this case, the doctor uses strong anti-cancer medications to kill cancer cells. Higher doses of chemotherapy are used to control advanced level cancer that may not be curable. But certain chemotherapy drugs could cause infertility and early menopause in premenopausal women. The ailment can also be treated with a vaccine known as servaris.
However, in all cases, cervical cancer must be detected and treated early because when the ailment is detected at a later stage, it is nearly always fatal. Experts warn that unless the Nigerian government acts fast by introducing measures for prevention, early detection and effective management of cervical cancer, the nation will continue to record greater incidence of death of women in their prime from the disease.
[divider]